
Dr Death and The Red Queen’s Race

By the start of 2003 it was becoming clear to me that things would have to change. Chris was seriously unwell, and getting worse. Trying to run a successful research group, give lectures, run a teaching laboratory, etc, etc, was in itself a demanding full-time job. Over which hung the stress of knowing that if I failed to get a new grant or contract we might lose one of the group’s members and our ability would then reduce. This had already happened when Duncan Pryde left after his funding ran out despite his project needing to continue to collect data for the Radiocommunications Agency (RA).
However my main concern was for Chris, trying to do more than simply ‘cope’ with her illness, and to actually help her to get better - and, indeed to survive! As a result I was finding that I was in a “Red Queen’s Race” situation where a failure on my part could end up being a matter of life and death! I was required to go to work to teach or see people there, but needed to be at home with Chris, and spend time with her not working because she desperately needed my support. But I simply didn’t have enough time or energy to everything as well as was needed. Alas – unlike Lewis Carroll’s Red Queen – even doing everything I could wasn’t enough. Chris was deteriorating, my research work was suffering. And when push came to shove, Chris mattered far more than the work!
I’d gradually shifted to spending more time at home and less in the Physics Dept. So far as was possible I was doing my own analysis work, writing, etc, at home, and discussing things with group members by email if I couldn’t leave Chris to meet them. I adapted this from day to day depending on Chris’s condition. As before she would go though periods of days or weeks when she found it difficult to get up or do anything. Being depressed, confused, and frightened, waking up at 3 or 4 am in a confused panic, etc. This was often accompanied by uncontrolled jerking or shaking, inability to concentrate, or simply being depressed, sleepy, or any combination of these symptoms. Her condition tended to improve during the day, but the same pattern would begin again the following morning like a predictable treadmill. Her fits came in bursts - sometimes as many as 8 to a dozen over two or three days, then none for a few weeks. Some fits were like confused, terrified screaming in fear, panic attacks for reasons she couldn’t explain afterwards, or often even remember.
January the 1st was a particular example of extreme behaviour. She kept following me around the house demanding that I explain why she should not dispair and kill herself. I kept trying to reply but everything I said was batted away or dismissed. It ended up with me locking myself in the bathroom to get away from her as she shouted at me through the door. But by the evening she was apologetic and admitted she wasn’t sure why she had behaved that way or exactly what she had done. And after a few days or weeks, these problems would fade away and she would be OK for some time... only to fall into another ‘down’ again some weeks or days later. Deja Vu, all over again!
As this kept happening gradually I decided that I could no longer cope. Chris was the priority, so I had started thinking about either taking early retirement or working part time. Members of my research group, the departmental secretaries, and Head of Dept, already knew about the difficulties and were sympathetic and helpful. So I began some informal discussions about the idea of retirement, etc.
Despite the problems we still usually managed to go out in the evening a few times per month for things like a meal at the Vine Leaf, or a show at The Byre theatre, or a concert organised by the St Andrews Music Club. Chris often felt much better by the evenings. And we did still tend to go to a Scottish Country Dance class on Sunday afternoons reasonably often. Although I kept having problems with the knee I’d injured a few years earlier and was a truly hopeless dancer we did enjoy the classes.
During January 2003 Dave Eden at the RA suggested that we might set up a new ‘CASE’ research studentship and have the student operate the 3-port interferometer and collect the atmospheric data for the project they had been funding. Unfortunately, the rules for co-operative research studentships had changed and getting one was now far more difficult than it had been. So this idea came to nothing. This was a disappointment because now that Duncan Pryde had left I was having to collect and process the data from the instrument about once a week, then send off copies of the results to Dave and to John Goddard at the Rutherford Lab. Which was another task which took me away from being with Chris...
On the 3rd of February we were shopping in Marks And Spencer in Dundee and Chris had a spectacularly serious fit/panic attack at about 11:45am where she kept cowering and shaking and screaming out that she was terrified – but could not say what frightened her or why. Nor could she understand what I said to her. This wasn’t the first such attack, so I did what I could to calm her down, but it clearly alarmed the staff and other shoppers despite their typically British reactions of not wanting to make a fuss. Chris had an appointment with one of the GPs in her medical practice at 3:40 that afternoon where we explained what had happened. I went with her so I could describe the events that morning.
For reasons which which will become clear later on, we did eventually get a copy of Chris’s medical notes for this period. Reading their content was a real shock because so many of the scribbled notes by the GPs involved bore little relationship to what had been said and often had no value in terms of any diagnosis or treatment. On this occasion the notes included the comment:
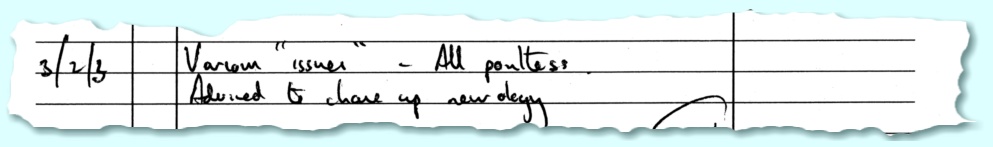
|
| 3/2/3 “Various "issues" - all pointless” |
It is hard to know how a later GP might use that to form a sensible diagnosis decide on treatment, etc. It gives no details at all of what was said, nor of the events of the morning. It simply seems to dismiss the patient as being s bit of a bore. Sadly, as later events were to show, this actually confirmed one of Chris’s greatest fears/anxieties – that no-one really understood how she felt, nor cared, not even wanted to help her. So that her situation was hopeless and she might as well kill herself! At the time, though, when they talked to Chris her GPs generally seemed to be sympathetic even though they didn’t seem able to suggest anything that would help beyond the occasional, “here try this!” approach to medication.
It had however, been arranged that Chris would be admitted to Ninewells for a few days of ‘observation’. We had been told that she would be monitored 24/7 by nurses and her behaviour and state observed continually. In particular if she had a fit or behaved strangely they would do an EEG and other tests while observing the seizure to try and obtain data that could aid diagnosis and guide treatment. So we had some hopes that this would prove a valuable exercise.
Over the weekend of the 1st and 2nd of March Chris had 3 fits, with another on the 3rd. She began her stay in Ninewells on the following day. She was put into a bed in a room and told to stay there and call a nurse if she felt a fit coming on. On the Tuesday she had two fits, each time calling a nurse. They came, and then went away again. So far as she could tell no EEGs were made, nor did a consultant ever appear. She remained there ‘under observation’ (sic) for the rest of the week. On more than one occasion she asked a nurse if she could see the consultant. They would tell her they would go and ask. They they would leave... and not come back. No consultant. No response.
I visited her each day, and could see that she was getting more depressed. It was bad enough that she was being left alone in a room with little to do and no-one to talk with. Add that to the failure to do any EEG or other tests or even see any consultants, etc, and it confirmed her underlaying anxiety that no-one really cared or felt they could help her. So nothing positive came out of the promised ‘observation’, only a confirmation of her worst fears that her situation was a hopeless one which no medic was even interested in helping her with. While she was in Ninewells I saw Janet Mackinnon, who was the University Occupational Health Advisor to discuss my own medical/work situation. This was one of a number of meetings I would continue have with her over the following months. The initial aim being to assess my health and fitness and see if she and the University’s GP could help me to cope with the situation and be able to continue work. Or, if not, to assess what might need to change – i.e. if I needed to either switch to part-time employment or retire.
On the 18th of March Chris saw her Neurology consultant at Ninewells. For reasons that will become clear later I will call them the “Red Queen”. Chris explained what had happened to her, including the worse-than-useless ‘observation’ period. The Red Queen’s reaction was essentially to keep saying Chris should see a psychiatrist. However it was arranged that Chris would have an MRI brain scan, in particular to examine her temporal lobes, on the 28th at Ninewells. Chris continued to feel particularly bad during this period after the non-‘observation’ and had another burst of fits, including ones in the night.
The scan took place on the 28th. At the time she found that they used some flashing lights that gave her a headache. The report on the scan came to us in April. This said that the scan “...shows some changes similar to those reported in 1996. However you also appear that you may have had a small stroke in the left posterior parietal/occiputal region. I would not have expected this to have made very much difference to your memory”...
Given the previous history of events we knew full well that Chris had indeed had a stroke a few years earlier. But no mention was made of the possibility that this might affect our real concerns about her depression, anxiety or confusion.
On the 1st of April Chris saw another GP. As was common at the time, I did not go in with her as I wanted to ensure she could speak freely and avoid the risk that she – or the GP – might think my presence was preventing her from saying what she wished. So I would only go in with her if she wished me to, or I could describe events she couldn’t recall because of a fit, etc. Chris came out and said that she’d only been told by the GP that there was “Nothing she could do!”. i.e. The GP offered her no hope or treatment at all. Which, of course, simply intensified her feeling that they neither understood, not cared, and had no interest in helping her. Again, when we later got a copy of Chris’s medical notes we found that the GP had written:
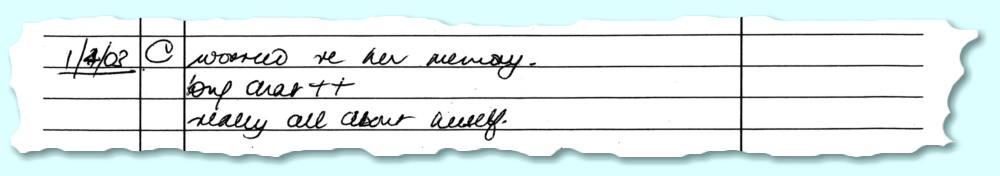
|
| 1/4/03 “Worried re her memory. Long chat ++. Really all about herself” |
Which does seem to confirm what Chris told me at the time about the ‘help’ (sic) she got from the GP. And on the morning of the next day Chris woke up early in a desperate panic feeling helpless and angry. We did manage to get out and do some shopping in Dundee later that day. But Chris remained depressed and anxious, and I was feeling really unwell due to stress and anxiety about her condition and the failure of the GPs, etc, to even offer any help.
One suggestion that had been made some time earlier, though, was that Chris should try a psychiatrist or therapist. So we found the details of one who offered therapy from a location in Hepburn Gardens in St Andrews. Chris then saw her a number of times during the next few months. I went with her on the first occasion so I could explain some of the details Chris would not recall – e.g. her behaviour during fits which she would forget afterwards. After that, I accompanied her when going and coming back, but she saw the therapist without me so she could speak freely without distractions. Unfortunately, although it helped in terms of being able to talk to someone who was sympathetic and clearly wished to help, it didn’t really improve things. So eventually she ceased seeing the therapist.
Over the weekend of the 5th/6th of April Chris became frantically anxious and frightened in the mornings and talking about killing herself, etc. I panicked and dialled 999 to get an ambulance and the police. They came and were with us for a while, then left again once we had both calmed down. The following week was awful as both of us were in a state of high anxiety and Chris kept waking up in the early morning, experiencing uncontrolled jerking movements, memory problems, etc. My levels of stress had now started to affect my eyesight. I had difficulty seeing and focussing my eyes, and also bright sunlight was painful and blinding. So I had taken to wearing glasses that darkened in sunlight and some clip on sunglasses when outdoors because otherwise I could not see where I was going and it was painful. On Tuesday 8th I signed off ‘sick’ from work for two weeks partly because I was unwell, partly to be able to stay at home with Chris because I was frightened about what she might do if I were to leave her alone for very long.
On Thursday 10th April I saw Stuart Pryde who visited me at home at 3pm. Stuart was working for the Fife Family Support Project (FFSP). This had been set up to help the families of those who had serious mental issues like clinical depression, bipolar disorder, etc. So we had been put into contact them. As a result I began seeing Stuart on a regular basis, and found this very helpful. By the following Sunday things had improved to some extent and we did get to the Sunday Country Dance Class, although we only danced a couple of times. The situation continued to be OK for the following week or two. At Easter we were able to do as we had in previous years and cook half a Turkey as a special dinner. We had taken to doing this because even the smallest turkeys sold for Christmas by Murray Mitchell’s (then the excellent butchers in St Andrews) were too large for us to eat at Christmas. Indeed, we would have struggled to get one into our small oven! So they would cut it into halves before delivering to us. We would then freeze one half for an Easter meal.
During the first couple of weeks of May 2003 Chris’s condition was such that she was able to get up and be active and interested in things. But during the week starting on the 19th she had a number of fits and her condition deteriorated again. She became anxious, confused, and in a state of panic for an increasing part of each day, with growing severity. Waking early and experiencing uncontrolled jerking movements, forgetting what she had just done, etc. Once again she repeatedly said she wanted to be dead and to commit suicide because no-one could understand and the doctors neither cared nor wanted to help her. On the morning of the 30th of May I became terrified that she would kill herself so I phoned the GP practice, explained, and asked for someone to come and see her as soon as possible.
This was the day that Dr Death came to call...
The front door bell rang and I went to open it leaving Chris in the living room. Although it was mid morning Chris was still in her nightware because she hadn’t felt able to get dressed. I opened the door and it was a GP that – so far as I can recall – I’d not seen before. He came in and I tried to welcome him and explain the situation. However he walked straight past me having seen Chris in the living room. Without asking either of us any questions or us having said anything beyond my “Come in.” at the door he marched up to Chris and said:
“There is nothing wrong with you. You and your husband have just had a ‘tiff’. There is nothing we can do for your anxiety, your depression, or your epilepsy. If you want to commit suicide you are perfectly free to do so.” |
I heard this as I walked in from the hall into the living room and I was stunned by his behaviour. I tried to explain that Chris was desperate for help, and the lack of even the promise of help was what was making her feel hopeless and hence suicidal. He ignored this and turned to me and said:
“You say that you are frightened to go out in case your wife commits suicide. I am telling you to go out and let her do as she chooses.” |
I tried to object to this and ask for help. However Chris was now feeling really desperate. She had been banging her head against the wall in anxiety, saying this was what she was doing to try and make the fear stop. She she didn’t want to kill herself but kept feeling there was no hope and that she would. Dr Death’s response was:
“So what?” |
and made plain that he didn’t care what she did or said, it was of no interest to him. She then grabbed his shirt front, pulled and shook that, desperately begging him for help. His reaction was to say:
“You have assaulted me! I will go back to the practice and have you removed from our list.” |
He then marched out again, ignoring anything I said. As he walked out Chris went upstairs. Having closed the front door I went up and found that she had got back into bed and was laying there. She did not want to talk to me. She said she just wanted to sleep. So I came downstairs for a while.
Because I was in a state of anxiety and bewilderment about the incomprehensibly callous behaviour of the GP I am not sure exactly how long his ‘visit’ was. But I doubt it was much more than a matter of minutes from start to finish. Throughout, apart from the ‘assault’, Dr Death was impervious to what either of us said or did and had no interest in listening.
During the next hour or more I’d go upstairs every now and then to check on Chris, and she would say she just wanted to stay in bed and sleep, not see anyone or talk to me. Since the general pattern was for her condition to improve as the day wore on, I accepted that and then would leave her alone for a while before checking again. However later on when I checked I realised that she had become rather more drowsy and confused and had been hard to wake up. I looked in the bedside drawer, and discovered that she had taken all the pills that had been there, and she admitted what she had done. So I rushed downstairs and dialed 999 for an ambulance. She had taken Dr Death’s ‘expert advice’... The ambulance came and took us both the Ninewells A&E. Chris was put under examination there and treated for her immediate symptoms.
The following was written by Chris as part of her account of what she could recall a few days later:
“After the doctor left on 30th May I accepted his suggestion and took a large overdose. Jim assumed I was taking a long nap. I remember very little about my stay in Ninewells except a conversation with a nurse in the middle of the night. She said she had two friends who had managed to live normal lives with Manic Depression. I have no memory of the time Jim had to wait until he was told I was not going to die and they found me a bed. I have no memory of the [Ninewells A&E] doctor who really impressed him with the gentle and professional way he applied the means of washing out my body.” |
For some time prior to this I’d become steadily more convinced that Chris actually suffered from a form of Manic Depression (MD) or Bipolar Disorder (BD) . At first this was from observing the way her mood and behaviour swung from ‘up’ periods of being active, positive, happy, and capable to ‘downs’ when she was confused, disparing, terrified, and unwilling to face anyone or do anything. But the medics we saw tended to dismiss or ignore the idea. However when the A&E duty Psychologist came to examine Chris when she was recovering I outlined the history for him and said we suspected she had a MD. He agreed that the history made this quite a likely diagnosis. This was a huge relief to me and I asked if he would write to Chris’s GPs, and her consultants, etc, to give them his opinion that this was the case. He said he would, and events later showed that he had done so. The following day Chris was transferred to Stratheden Mental Hospital and spent the next four days there to recover whilst being observed and assessed.
Although it was a truly awful experience that should never have happened if Dr Death had done their job correctly, the opinion expressed by the A&E medic was a significant step as at last we had a relevant medical opinion which others would now have to consider, not simply wave away. That excepted, the entire episode seemed then, and now, like the kind of nightmare that you might assume could only appear in overly-dramatic fiction. But in stark reality, it really happened to us, and was nearly the end of the story for Chris. Doctors bury their mistakes!
When we obtained Chris’s medical notes later on we discovered that Dr Death’s official record of their visit can perhaps, best be described by a phrase sometimes used about politicians and civil servants who would give an account that is, erm, “economical with the truth”! In this case, Dr Death’s account of his visit was as follows:
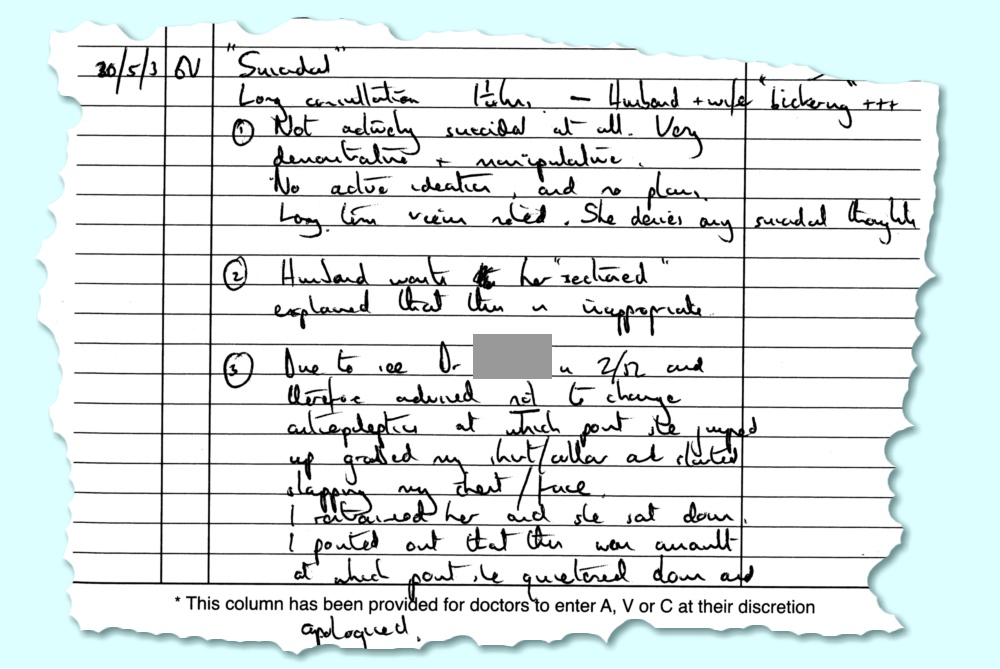
|
|
“ "Suicidal" Long consultation 1¼ hours – Husband + wife "bickering"+++ (1) Not actively suicidal at all. Very demonstrative and manipulative. No active ideation and no plans. Long term views noted. She denies any suicidal thoughts. (2) Husband wants her "sectioned". Explained that this is inappropriate. (3) Due to see Dr XXXXX and therefore advised not to change antiepileptic at which point she jumped up grabbed my shirt/collar and started slapping my chest/face. I restrained her and she sat down. I pointed out that this was an assault at which point she quietened down and apologised.” |
The reality was starkly different. Chris had repeatedly said she felt suicidal and was desperately asking for help to stop her killing herself because she felt her situation was hopeless and no-one understood and would help her. Alas, the GP flatly refused to help and essentially confirmed her fears. The assertions that she was “Not actively suicidal”, etc, are demonstrably untrue as she had actually taken an overdose and tried to kill herself shortly after the GP left – as directed by Dr Death’s ‘advice’ – which curiously doesn’t get mentioned in the notes. From this it is also obviously untrue that she denied any suicidal thoughts. In fact she was repeatedly begging the GP to help her to overcome them and offer her some hope.
The “bickering” was my trying to explain to Chris and the GP that she needed help, not to be told to go ahead and commit suicide. That was the key reason I had phoned for a GP to come. She had been sectioned in the past, and had attempted suicide, but Dr Death’s behaviour and notes show no sign of being aware of this. What we both were wanting was treatment to be changed to try and deal with the bigger problem of depressions, anxiety, etc, that were driving the suicidal thoughts and feelings.
The comment in the notes about changing the antiepileptic (medication) again totally fails to understand what both Chris and I were saying. We were both trying to explain that in practice her suicidal feelings, etc, were a far bigger threat to her life and condition than her fits. So that a change of medication of some kind might well be beneficial and should be considered. But again the notes show a failure to listen what we both had said. Demonstrating that Dr Death’s mind had been made up before I’d opened the door. Fortunately, Chris’s medication was changed after this terrifying episode, for reasons that had nothing to do with Dr Death’s opinions, or notes.
She did not slap the GPs face, etc. This is simply untrue. She did grab Dr Death’s shirt and try to shake it, frantic to get the GP to listen, understand, help her. But all she got was the ‘advice’ to kill herself if that was what she wanted. ...Oh, and I doubt the “consultation” lasted anything like as long as claimed in the notes. But for all I know, Dr Death went and had a cup of coffee to relax after his visit because he had found it a nuisance. Perhaps also give him some time to compose his story when he had her removed from the practice.
It also evident that Dr Death’s notes must have been written some time before finding out that Chris had actually promptly taken the ‘advice’ they’d given to her. Indeed, Chris may well have been on the way to Ninewells, or in A&E there as the notes were written. However we didn’t see the notes until some months later, so at the time we did not know what Dr Death had written. That discovery came later on...
We duly received a letter dated 12th June from Dr Death’s practice which was explicit that Chris was being removed from their practice list, commenting that: “...although we understand that it is and [sic] emotional and difficult time for you, it is always unacceptable to physically assault a Doctor.” A point which both Chris and I agreed with. However given the circumstances, it must take some brass neck to call it an “assault” when she was being told to kill herself by a GP we’d called to help her! A few days later we received a letter dated 16th June from the Practitioner Services division of the NHS. This told us that Chris would be removed from Dr Death’s practice list on the 24th of June. It stated that the GP was not required to give any reason for removing us from their list. We then registered with a different St Andrews GP practice. (For obvious reasons, although I’d not been removed by the practice I wanted nothing to do with them after what had happened. I thought it better for Chris to switch with her – and probably safer for me in the long term given the ‘standard of care’ Chris had experienced!)
We did briefly consider making a formal complaint about Dr Death’s behaviour but decided it would probably be at best a waste of time and effort. In practice it would be our word against Dr Death’s. In the circumstances, neither Chris nor I were in a state of mind able face a stressful battle over the episode. We wanted to focus on keeping Chris alive and actually get help and treatment of an appropriate kind. Trying to argue a case against Dr Death would have made her situation worse, not better. We did write and send a letter to the practice later on, stating what we had experienced, so that would at least know, even if they ignored it. But we also said that we would not make a formal complaint. Quite simply, from our point of view it was a matter of the old phrase, “Good riddance to bad rubbish” – a feeling intensified when we saw the medical notes later on. I can only wonder how other patients with serious medical conditions were treated by Dr Death and hope they all managed to survive the experience.
The good news, eventually, was that a change of GP practice, and finally finding some support for the idea that Chris had Bipolar Disorder was eventually to prove a game changer. Although sadly, it was to be a slow and erratic uphill struggle for some years to come and during June both of us continued to be seriously unwell.
One curious point about the medical notes for this time, though, is that there is a gap in the GP notes between 30th May and 3rd of July. Usually, when either an Ambulance was called to attend Chris, or she was taken to Ninewells or Stratheden there would be a printed slip summarising the details in the main notes. But there was no such note in the pages we were shown and copied. Which does make me wonder if this was, erm, ‘omitted’ because it would have been embarrassing for Dr Death and their practice to have it directly follow below what Dr Death wrote about that day, by flatly contradicting it with mere facts.
The next few weeks were pretty difficult for both of us. I kept telling her that things could and would get better in time. And that we would eventually find the right treatment and make any necessary changes to help her feel better. The change of GP practice, the comments by the psychologist who’d seen her in Ninewells, and the response and support from the FFSP all pointed in that direction. By this time each of us was seeing a (different) support worker from the FFSP and they were helping us to get a clear and appropriate diagnosis along the lines of Bipolar Disorder as they recognised the symptoms very easily given their experience.
Unfortunately, Chris was very reluctant to believe anything would change for the better. Dr Death had firmly confirmed her worst fears that none of the medical people cared or would help, and they would prefer her to die so they could forget about bothering with her. She remained anxious, confused, with the usual set of symptoms including uncontrolled jerking movements, tiredness, forgetfulness, etc. I continued to be stressed to the point of having a headache or being dizzy and out of breath a lot of the time, and continued to have problems with my vision. Most of the time I avoided going to the Physics Dept unless I had no alternative. I needed to stay with Chris both to help her and because I was worried about what she might do if I were out for too long. Almost as a background process, we got the details of her Dad’s probate process from the solicitors, reminding her that her father was now dead.
However as the weeks passed she gradually seemed to come out of the ‘down’ and things got better. With her agreement I gradually resumed going out to work a bit more often. On the 20th of June the Head of the Physics Department agreed with my suggestion that I should take early retirement of some kind to reduce my commitments. Both to reduce the pressure on me, and to let me spend more time with, and helping, Chris. The suggestion was that I essentially cease any research, but might do a modest amount of part-time teaching work. That could serve two purposes: It would give me something to do that helped distract me when things were difficult, and it would also gradually tail away my teaching and give the Department time to ease other people into taking over my teaching duties.
So I initiated a more formal process of trying to agree the details of my eventual retirement. During the following few days Chris’s behaviour and mood improved and she became quite cheerful and active. She insisted that she was now OK and wouldn’t try to kill herself again. As a result I also felt better and decided that she had now realised that things could and would get better. Or that at least she was now in a ‘up’ phase and was more confident and active. I became more relaxed about leaving Chris by herself, and started going to the Department more often, for a bit longer.
On Monday 23rd of June I came home and entered the house, calling out to let Chris know I was home. I got no reply so I walked around from room to room becoming more and more anxious as failed to find her. When I went upstairs to the bedroom I found a long suicide note on the bed – but no sign of Chris! I panicked at this point and ran about the house and then into the street screaming out her name in the desperate hope she would hear me and answer. But got no response. I then ran back in, dialled 999 to call the police and reported what I’d found. Having done that I also phoned the local taxi firm, Williamsons, asking them for help. This was because they, and their drivers, had got to know us both quite well. We regularly use their taxis, and they’d also often carried Chris home from hospital as well as took her to and from the various meetings she’d attended over the years. They said they’d alert all their drivers to keep an eye out to see if they could find her as they went around the town.
The police then arrived. I explained the situation and showed them the set of A4 pages of suicide notes that Chris had left. They searched the house and then outside. One of them said he had heard a noise from our garage. I’d run outside, and also to our back garden when I’d gone out screaming for her, but hadn’t thought of the garage which is separate from the house. We opened the door and found her in the dark, laying on the floor in a pool of blood. They called an ambulance which came and took her to Ninewells. She was alive, but in an awful state. She had badly cut her head which was covered with blood.
Once again she had attempted suicide. Her increasing cheerfulness had actually been because she had decided to kill herself and felt confident that this time she would succeed! She had carefully planned how to do it, and decided to wait until I was happy to go out for long enough that I would not be able to discover the attempt until it was too late. So once I’d gone out on the 23rd she proceeded to take an overdose of her medications. She then drank a lot of brandy and went out to the garage. She took with her some sticky tape, a peg, and some metal skewers. She taped up her mouth and put the peg on her nose to try and stop herself from breathing. The next step was meant to be to push the metal skewers into an electrical socket and electrocute herself! The intent being that if she used a number of methods then at least one of them would work, and kill her!
Fortunately, in some ways, the attempt was like a sick farce. By the time she had taped up her mouth the combination of the overdose and the brandy had made her very muddled. She had closed the garage door to hide that she was there. When she then wanted to use the skewers to electrocute herself she had to pull out a mains plug to access the socket. However the plug provided the power for the lights, and pulling it out plunged her into darkness! In her drunken state, she was unable to see well enough to insert the skewers. She then dropped them and must have stumbled about in the dark for a while. By the time we found her she had fallen over some glass, broken it, cutting herself badly as she did so! It isn’t clear how long she remained there, but she was then found on the floor of the garage in that state – thankfully still alive but alarmingly covered in blood!
She was treated in Ninewells and they agreed to discharge her the next day. The cut on her head required five stitches. The episode was a real shock for me because she had for days beforehand presented such a ‘false front’ of being OK, when in reality she was happy because she had decided how to die and was getting me to going out so she could do so. Following on from the attempt I wrote a letter to her consultant, Dr Neilson, at Stratheden Mental Hospital asking for an urgent early appointment to see her, detailing what had occurred. I also stressed that we strongly felt that she needed help on the basis that we felt that she was suffering from a serious case of Bipolar Disorder (BD) or Manic Depression (MD). In particular, we wanted people to recognise that this was now the most serious threat to her life and condition, not her epilepsy. It also underlined in my mind that it was vital that I should reduce my University workload and retire to be able to spend more time with her. However things remained difficult because she was unhappy about having failed in her attempt.
Chris had a planned meeting with Dr Neilson at Stratheden in August. However he replied promptly and set up a new appointment for the 2nd of July. Chris also saw a GP from her new practice for the first time on the 2nd. The stitches for her head wound were removed on the 4th. Unlike Dr Death and Chris’s previous GP, Dr Neilson and her new GPs were willing to take seriously the idea that Chris was, indeed, suffering from a serious form of depression/BD/MD. As were the support workers we were now both seeing. This was a significant advance, but Chris remained seriously unwell despite the hope this offered for the future.
We had also put in a formal request to see Chris’s medical notes. As a result we saw these, and copied some of them, on the 23rd of July. That was when we were shocked to see what the GPs in her previous practice had been writing about her. It became evident that for many years they had pretended to be sympathetic and helpful, yet hadn’t actually listened to, or understood, what she was going through. The notes made by the GPs in her old practice were virtually content-free in actual medical terms! As a result, their ignorance propagated as later GPs would read the notes and form a totally incorrect, and seriously damaging, impression. In contrast, the few notes made by her new GP during July were entirely different and dealt with real issues and possible treatment options.
The initial suggestion by Dr Neilson was that Chris should try taking Lithium because this was a commonly effective medication for stabilising the mood of people who have BD. I did some research on the matter and was surprised by what I discovered. Again, this was a consequence of having been mislead by Chris’s old GPs. I had asked them about having Chris try taking an antidepression medication of some kind, if only because she was clearly suffering from bouts of severe depression. They had rejected the idea. I was repeatedly told that this was counter-indicated by epilepsy because it carried the risk of making fits more common and/or severe. However a side-effect of the way her old GPs had failed to help Chris had been that I had increasingly taken to doing my own research on relevant medical matters...
The initial discovery I had made that way had been some time earlier. I was reading medical journal papers on topics like depression and anxiety because these were frequent symptoms Chris exhibited. I then came across some papers on Bipolar Disorder, etc, and found one that listed the symptoms. At the time I had heard the term ‘Manic Depression’ if only because it was the title of a song by Jimi Hendrix! But I had no idea clear what it involved. As I read down the list of symptoms, on seeing each item I said to myself, “Yes”, “Yes”, “Yes!”, “Oh yes!!”,... all the way to the bottom. As I did this I could feel – and again do now, while I write about it – a feeling like icy fingers running down my spine as I realised this was what was crucifying Chris. A weird mix of relief at seeing clear evidence confirming what was wrong, and horror at the confirmation. However, when I’d repeatedly suggested that Chris might suffer from MD to her old GPs they had dismissed the idea. And insisted she could not take medication for this because of her epilepsy.
When I did some research to consider the proposal for Chris to try Lithium I discovered that the reality was rather different. Some medications were routinely given for both epilepsy and depressive conditions. Discussing the situation with Chris we also agreed that the margin between a beneficial dose and an overdose of Lithium was narrower than we felt comfortable given that she did get confused or upset at times. So having looked at the literature we suggested that Chris be prescribed Carbamazepine rather than Lithium, and Dr Neilson agreed.
During the last few days of July I exchanged some emails with Mark Evans who had now moved on from his job at DERA Malvern and was completing his PhD thesis. He had begun this with me acting as his Academic supervisor, but because I was having to take so much time off, etc, I had arranged with Graham Smith for him to take over as Mark’s supervisor and deal with Mark’s viva examination which was approaching. I was still coming into the department each week to transfer data from the 3-Port system, process it, and post CDROMs of the results to Dave Eden at the RA and John Goddard at the Rutherford lab. However apart from this, my personal research work in physics had essentially ended by the the middle of 2003. I was carrying out my undergraduate teaching as best I could, but spending as much time at home with Chris as possible. I was also developing additional physical problems with unpleasant symptoms that have continued to grow worse from then until now.
During the rest of July, August, and into September Chris saw a GP, and/or her Community Psychiatric Nurse (CPN) and/or a support worker almost every week. I also saw support workers and the University Occupational Health Advistor regularly, and kept discussing the arrangements and timing for my retirement with the Head of Department. We also went to meetings with various people involved with the groups that supported people and families suffering with Manic Depression, etc, and Chris – when she felt capable - would try to help with campaigning, etc. But a lot of the time she continued to suffer the familiar symptoms – anxiety, confusion, severe depressions, uncontrolled jerking movements, and her fits. Although we would often go out, a lot of the time she felt too ill and frightened to see anyone, so stayed at home, often in bed during much of the day. I continued to be severely anxious and stressed, finding that I often had no idea what to do because nothing I tried seemed to help, and just made things worse. We had made some progress in terms of recognition of the nature of the problem, but not with dealing with its effects. We had, at least, come to think that the NHS medical people we saw understood and were now wishing to help. Then Chris went to an appointment on Tuesday 23rd of September at Ninewells to see a Neurologist there who I will call ‘The Red Queen”...
When we went in Chris started to explain what had happened during the last few months and that she was still in a bad state of anxiety and depression after making more than one serious suicide attempt. As she was doing this the Red Queen started to laugh at her, clearly thinking what had happened and Chris’s state was absurdly funny! This horrified me and Chris was alarmed and panicked because it – once again – confirmed her deep fear that the medics neither knew nor cared and didn’t want to help her even if they could! She got up and ran out of the room, with me chasing after her. I managed to catch up and stop her, and eventually got her to come back to the consultation room. But she then didn’t want to say any more to the Consultant and the meeting ended shortly afterwards. The Red Queen didn’t attempt to make any kind of apology.
During the next couple of days Chris stayed at home and was very upset and depressed. I remained at home as much as possible. But on Friday 26th September I had to go to work for the first time since Chris has seen the Red Queen. I went out at about 10am and came home at about 1pm. I found that Chris had remained in bed, and was very difficult to awaken. When I did wake her she admitted she had taken an overdose to kill herself and had been waiting for me to go out so she could do this. She had written and left another suicide note. I dialled 999 and the ambulance took her on the now distressingly familiar route to Ninewells A&E. They kept her in overnight but let her come home the next day. We got home on the Saturday at about 3:30 in the afternoon. However Chris remained seriously depressed and in a state of suicidal dispair and confusion, so the next day I range the St Andrews Health Center. Someone came and spoke with her, and she was then taken to Stratheden again. They kept her in until Thursday the 2nd of October.
We can’t know, but can only suspect that the inappropriate and dangerously misleading ‘notes’ from her previous GPs may have been read by the Red Queen and led her to behave as shamefully as she did. However the result was, yet again, to confirm Chris’s fear that her only way out was to die. We wrote detailed letters to her new GP and to Dr Neilson, telling them exactly what happened. Later on we also wrote to Ninewells and made it utterly clear that under no circumstances should Chris ever have to see the Red Queen again, explaining why in stark detail. However – as with Dr Death – we felt it would simply make our own situation harder to try and make a formal complaint. Instead we just wanted Chris to be seen and treated by medical people who actually knew what they were doing and how treat her appropriately.
Much later, on the 10th of October, we received a very brief letter from the Red Queen making what I can best describe as a ‘vague almost-apology’. In total it said:
|
“I am writing to apologise for being somewhat insensitive this morning. I appreciate that you are having significant problems and I am doing my best to try and find some way to help.” |
The letter was dated 23rd September. but only arrived weeks later – well after we had written to others describing what had happened. The content does remind me of the ‘non-apology’ letters that politicians tend to write using phrases like, “I am sorry if you were offended” rather than admitting they made a serious mistake. However you look at it, for a person in the Red Queen’s position and field the phrase “somewhat insensitive” seems in itself to show a serious lack of understanding. It reads like a letter which they have been told to write, whilst actually admitting nothing specific. No-one reading it would be able tell how shockingly inappropriate the Red Queen’s behaviour had been, or its consequences. We were, however, told indirectly much later that the Red Queen had been send on “gardening leave” for a long period. Although we have no idea if that was a direct result of how the Red Queen had caused Chris to make another suicide attempt, or if there were other incidents.
I have chosen the name “Red Queen” because I do wonder if they, along with Chris’s old GPs were victims of a state of mind which I fear it may be all too easy for medics to fall into.
Just as I had been finding I was trying to run a “Red Queen’s Race” to keep up with all my University work and help Chris, so I fear that many medical people in the NHS may become so busy just trying to keep up day to day with their work that they can easily drift into sort of mechanical approach. Patients get pigeonholed and from then on are treat treated on the basis of the label on that pigeonhole. Symptoms get confused with causes and the ‘cause and effect’ chain either reversed or missed. Any signs or symptoms that don’t fit are simply ignored. If that then means they also don’t appear in the medical notes, the pattern becomes set in stone.
This all may be understandable, but it is unforgivable when it gets to the point of letting professionals openly laugh at desperate pleas for help, or tell the patient to go ahead and kill themself! Whatever the reason, it makes me wonder how many people’s lives are ended or ruined by such gross failings on the part of medical people who really do need to know better. But of course, doctors bury their mistakes, and dead people can’t read their medical notes! Whatever the reasons, 2003 was a truly awful period for Chris and myself, made far, far worse by how Dr Death and the Red Queen behaved.
During the first week of October Dr Neilson and Chris’s new GP set about arranging ‘multi-agency’ support for Chris and considering ways to decide how best to treat her condition. Things did – gradually and erratically – begin to improve after this, but it took more years that it should for Chris’s problems to be recognised and for relevant support and treatment to be provided. I can only wonder about to what extent we were lucky, and to what extent it was because I was bloody-minded enough to keep looking for the correct diagnosis and treatment and arguing with the original GPs, etc because I was determined not to lose Chris as a result of their lack of care or concern.

To put 2003 into medical context I assembled the above illustration a few years later. It shows when she had a stroke, and when the suicide attempts were made. It also shows a time-smoothed plot of the number of fits she was having per month, and some of the changes in her medication. In hindsight it indicates that the Keppra medication Chris tried for her epilepsy may have reduced the number of fits she was having. Unfortunately, it also gave her the serious side-effect of making her wrists and arms too painful to use. So had to be abandoned. It also seems to show that her brief use of a beta-blocker was a bad idea, and triggered the stroke. In addition it also looks like the HRT we though might help her mood wasn’t really doing so, and may have actually led to an increase in the number of fits. But it is hard to untangle that from other changes like the use of Keppra. The details of her medication history were more complicated than shown in the graphic because it was often altered to see if a change might improve her condition. However the main relevant alteration here was to gradually shift from Lamotrigine to Carbamazepine because it was felt that the latter would prove better with regard to her Bipolar condition.
Looking ahead from 2003, though, it shows that Chris did not make any suicide attempts in 2004 which was a big improvement, although she continued to be seriously unwell. The problems in these later years was to be finding and maintaining the optimum treatment. This was a slow and difficult process for reasons that people who have no direct experience of Mental Health issues may not realise. Quite simply then – and now – Mental Health is one of the ‘poor relations’ of health care in the NHS and for Local Authority care services. In medicine if you want to become a prominent and wealthy consultant held in high regard, the fields to concentrate upon are ones like brain surgery or cancer. In comparison, mental health and care of the elderly tend to be underfunded and something most people don’t even like to think about, let along ensure are well funded and researched.
A particular challenge is that people often tend to fear or feel uncomfortable about mental illnesses, so prefer not to think about them at all. And the symptoms often “make no sense” and seem baffling. The tendency to react with a “pull yourself together” attitude tends to come into play. In a way this is understandable because if you don’t suffer from such problems what people who have them say or do does indeed, “make no sense” – but that’s why they are symptoms of a genuine and serious problem they need help to deal with. The illness is a real as a broken leg, but not so easy to point at and then supply a simple ‘cure’. For professionals there may be no status or gold in the area, and they may not know what to do. For others, the confusion, embarrassment or perhaps fear often evoked can drive people to avoid even thinking about it. As a result, the qudos, attention, and the cash go to elsewhere...
Despite having initially been his supervisor, by the time it came for Mark Even’s PhD viva I wasn’t up to taking part. But at the start of October I was pleased to be able to congratulate him on having been awarded a PhD, and apologising again that I’d not even been able to be in the department when the examination took place. Chris – and I – had at the time simply been too unwell and preoccupied with the way she had been treated.
On the 22nd of October I sent a format request to the University asking to be allowed to take an early retirement, subject to sorting out the relevant details. This was accepted, and the process then began. The only form of mm-wave ‘research’ I was doing by this time was that I continued to go into the department about once a week to process and send off 3-Port atmospheric data to the RA and Rutherford Lab. Essentially all the other research was now being done by Duncan Robertson, Graham Smith, Dav Macfarlane, and the others.
Dave Eden had been trying to get another research studentship running and have a student take on the data collection and processing. However this failed for two reasons. One was that the rules for studentships had been altered, making this harder for the RA to support. The other was that UK Government had decided to ‘merge’ the RA into ‘OfCom’. The politicians had decided that having a state funded research agency assessing and deciding on the best use of the UK radio spectrum was unnecessary. Instead this was to be left to ‘the market’. The idea being that radio spectrum was a salable asset and thus a source of funding for Government, not something to spend public money on. So in practice, the ‘merger’ was actually a death sentence for state support on the propagation behaviour of the atmosphere. Let the private companies decide, and then compete to pay up. As a result, in the end all the work I and others put into this project came to nothing because the large mountain of data collected was never really used – apart from a few presentations I gave to people showing interesting results.
On the 23rd of October Chris started to be seen by an Occupational Therapist on a regular basis. Over the following years the use of Occupational Therapy (OT) turned out to one of the more successful ways for helping Chris, so this proved to be a change for the better. She was now also seeing a Community Psychiatric Nurse (CPN) on a regular basis as well as her new GP about once a week.
Despite having to often take breaks from work, and either shift lectures or ask others to help, I did continue to do some teaching duties as best I could. In particular I continued to help run the Electronics teaching laboratory whenever I felt it was safe for me to do so. Lecturing was generally timetabled for the mornings when Chris was at her worst when unwell. Whereas the teaching lab was in the afternoon, and the work was shared. So it was easier for me to deal with than the lecturing.
The year finished well with Chris and myself both feeling cheerful and we enjoyed a turkey dinner that we prepared, cooked, and ate, together. We had survived! And to be honest I was now looking forwards to retiring and that making life easier for us both.
Jim Lesurf
10,000 Words
24th May 2020
Chris and I did survive though the following years and things – gradually – improved. We have since had many happier years together. The main reason I have written the above detailed account is that I fear that many other people who need appropriate help with mental health problems may be abused or mistreated by medics in ways as bad as the examples we encountered. If so, please know you are not alone. It is possible to get the right diagnosis and better support and treatment, but it may be an uphill struggle. Never give up as that way you let the bad medics bury their failures and move on! It can be a hard road, but the end goal is worth the effort. Nil Carborundum!